Medication Optimization on a Large Scale: Collab between Institutional Special Needs Program, a Medical Provider Group and a SNF Org
1.50 CME / 1.50 CMD Management / 1.00 MOC
This session will review medication optimization programs in the post-acute and long-term care continuum from the perspective of an ISNP, provider organization and nursing home chain and how synergy between the three partners can lead to large scale implementation. Details discussed will include deprescribing algorithms, medications targeted, and timing and frequency of deprescribing together with opportunities of leadership and operational support at each level.
Presenters
 Monica Ott, MD, CMD, currently serves as the Optum Complex Care Management (CCM) medical director for the Indiana and Oklahoma markets. Dr. Ott currently leads the Medication OPTUMization initiative and works with the education team on clinical topics for the advance practice clinicians such as COVID-19. She has been active in AMDA for many years and has a CMD. She previously served on the Clinical Practice Guidelines committee. Dr. Ott is a past AMDA Indiana chapter president.
Monica Ott, MD, CMD, currently serves as the Optum Complex Care Management (CCM) medical director for the Indiana and Oklahoma markets. Dr. Ott currently leads the Medication OPTUMization initiative and works with the education team on clinical topics for the advance practice clinicians such as COVID-19. She has been active in AMDA for many years and has a CMD. She previously served on the Clinical Practice Guidelines committee. Dr. Ott is a past AMDA Indiana chapter president.
 Michelle Graham, PharmD, BCPS, is a Manager of Clinical Pharmacy Patient Care at Optum. She builds and manages processes that improve member adherence and assists clinical staff with appropriate prescribing in our long term care and assisted living members. She manages a team of pharmacists and nurse practitioners who assist in these endeavors. She is Board Certified in Pharmacotherapy and serves on the Pharmacy Quality Alliance Educational Committee.
Michelle Graham, PharmD, BCPS, is a Manager of Clinical Pharmacy Patient Care at Optum. She builds and manages processes that improve member adherence and assists clinical staff with appropriate prescribing in our long term care and assisted living members. She manages a team of pharmacists and nurse practitioners who assist in these endeavors. She is Board Certified in Pharmacotherapy and serves on the Pharmacy Quality Alliance Educational Committee.
 Cathy Lipton, MD, CMD, is National Medical Director for Institutional Programs within Optum Complex Care Management. She supports the delivery of quality clinical care for Special Needs Plans focused on long term and post-acute care populations. Dr. Lipton has served on the American Health Care Association's Clinical Practice Committee and Professional Development Workgroup and is a Past President and long-standing board member of the Georgia Medical Directors Association.
Cathy Lipton, MD, CMD, is National Medical Director for Institutional Programs within Optum Complex Care Management. She supports the delivery of quality clinical care for Special Needs Plans focused on long term and post-acute care populations. Dr. Lipton has served on the American Health Care Association's Clinical Practice Committee and Professional Development Workgroup and is a Past President and long-standing board member of the Georgia Medical Directors Association.
 Sabine von Preyss-Friedman, MD, CMD, FACP, is an Internist and Geriatric Medical Specialist and has practiced in Skilled Nursing Facilities since her fellowship at the University of Washington in 1988. She first became a certified Medical Director in 1992 and has since been enthusiastically engaged in Medical Direction of Skilled Nursing Facilities. In 2011, she was honored by AMDA as Medical Director of the Year and in 2021 as AMDA’s Choosing Wisely Champion. As a Medical Director, she is involved in Quality improvement, developing standards and outcomes measures in our facility and the successful translation of medical evidence into clinical care. Dr. von Preyss-Friedman currently serves on AMDA’s board and as the president of the Washington State Society of PALTC.
Sabine von Preyss-Friedman, MD, CMD, FACP, is an Internist and Geriatric Medical Specialist and has practiced in Skilled Nursing Facilities since her fellowship at the University of Washington in 1988. She first became a certified Medical Director in 1992 and has since been enthusiastically engaged in Medical Direction of Skilled Nursing Facilities. In 2011, she was honored by AMDA as Medical Director of the Year and in 2021 as AMDA’s Choosing Wisely Champion. As a Medical Director, she is involved in Quality improvement, developing standards and outcomes measures in our facility and the successful translation of medical evidence into clinical care. Dr. von Preyss-Friedman currently serves on AMDA’s board and as the president of the Washington State Society of PALTC.
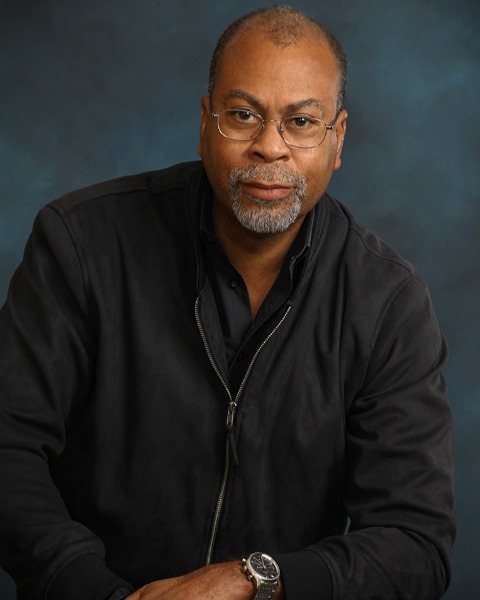 Jerry Wilborn, MD, FCCP, is CEO of GAPS Health (Geriatric Administrative Provider Services), outsourcing utilization management and utilization review to nursing facilities via best in class Medical Directors. Dr. Wilborn’s fellowship training in pulmonary and critical care medicine was also at the University of Michigan, where he stayed on as faculty doing basic science bench research. He has started and built out several successful post-acute practices, two of which were acquired by a publicly traded company. He has served as National Medical Director of the largest post-acute practice in the nation, a practice that staffed over 2000 nursing homes, 500+ assisted and independent living facilities, with over 3.2MM patient visits per year.
Jerry Wilborn, MD, FCCP, is CEO of GAPS Health (Geriatric Administrative Provider Services), outsourcing utilization management and utilization review to nursing facilities via best in class Medical Directors. Dr. Wilborn’s fellowship training in pulmonary and critical care medicine was also at the University of Michigan, where he stayed on as faculty doing basic science bench research. He has started and built out several successful post-acute practices, two of which were acquired by a publicly traded company. He has served as National Medical Director of the largest post-acute practice in the nation, a practice that staffed over 2000 nursing homes, 500+ assisted and independent living facilities, with over 3.2MM patient visits per year.
Learning Objectives
- Utilize an existing infrastructure to disseminate educational materials such as deprescribing algorithms, talking points, and examples of conversations with patients and/or families to improve the providers’ confidence and skill in deprescribing unnecessary medications.
- Discuss how and why optimizing medication regimens lead to better patient outcomes.
- Communicate the benefits of the medication optimization (e.g., to patients, patients’ families, PCPs, facility nurses, and clinical-support staff) to all post-acute facility stakeholders.
Credit Information
Activity Created 3/2022
Credits Available Until 3/2025
Credit Statements:
CME: AMDA – The Society for Post-Acute and Long-Term Care Medicine designates this enduring material for a maximum of 1.5 AMA PRA Category 1 Credit(s)TM. Physicians should only claim credit commensurate with the extent of their participation in the activity.
AMDA – The Society for Post-Acute and Long-Term Care Medicine for Post-Acute and Long-Term Care Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
MD: This self-study activity has been pre-approved by the American Board of Post-Acute and Long-Term Care Medicine (ABPLM) for a total of 1.5 management hours toward certification or recertification as a Certified Medical Director (CMD) in post-acute and long-term care medicine. The CMD program is administered by the ABPLM. Each physician should claim only those hours of credit actually spent on the activity.
ABIM Maintenance of Certification (MOC): Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.5 Medical Knowledge MOC points and patient safety credit in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program.
Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
Visit the Continuing Education page for information on if and how you can claim credit/hours for AMDA’s education.
Disclosure Information:
The Society requires the disclosure of all speaker/faculty/planner’s relevant financial relationships; presence of off-label use of a device or medication; and discussion of any experimental, new or evolving topic prior to each accredited education activity.
If the learner perceives any bias toward a commercial product or service, advocation of unscientific approaches to diagnosis or therapy, or recommendation, treatment, or manners of practicing healthcare that are determined to have risks or dangers that outweigh the benefits or are known to be ineffective in the treatment of patients please report this to the Society’s staff.
All relevant financial relationships have been identified, mitigated, and resolved.
- The following AMDA Education Committee members have financial relationships to report: Diane Sanders-Cepeda, DO, CMD — UHC E&I Retiree Solutions: Full-Time Employee; all others have no relationships with ineligible companies.
- The speakers have no relevant financial relationships.
- AMDA staff have no relationships with ineligible companies.